Mental health service users call for a fresh approach to the design of psychiatric care environments in hard-hitting conference session
Mental health service users have provided a damning insight into life on many psychiatric wards in the UK and are calling on architects, designers, and manufacturers to work with patients to create more-therapeutic environments.
Speaking at the recent Design in Mental Health Annual Conference held in Coventry, a number of patients with mental health conditions spoke out about the poor state of wards; with smells, a lack of privacy, noise, and the threat of attack from other patients among their concerns.
A lack of grounding
Kenita Watson, who has experience of being detained under the Mental Health Act and works as an advisor to the Care Quality Commission, told the conference: “At one hospital immediately on entering I recall the smell; a musty smell that did not remind me of anything – a totally-unique smell to this environment caused by bad ventilation and a lack of fresh air.
Mental health hospitals have been around for thousands of years, but the focus is on protecting infrastructure rather than people and that will take time to change, but it has got to happen
“It can feel surreal, and this is compounded by the lack of natural lighting.
“It articulated and exacerbated my lack of grounding.
“Bright lights shining through an observation panel in my bedroom door looked out onto a corridor where everything echoed like surround sound.
“And I was very aware of an incident taking place, but had no idea what was going on and it was not conducive to a good night’s rest.”
She added: “In the morning you try to shower, but it is on a timer and keeps switching off. My only previous experience of this was at a swimming baths and it reminded me of the lack of privacy.
“And when you try to spend time in public areas, there is no space and you can observe patients in crisis.
“I think it’s a general lack of understanding of how a small issue can be so big.
Relieving boredom
“For example, listening to music or being told we can’t charge our phones during the day. Being able to keep my phone was key for me.”
She also called for more private spaces, recalling visits from family members which took place in the dining room.
“This brought a lot of embarrassment as there was no privacy at all and my visits were interrupted by other patients, making my visitors feel uncomfortable, and I felt this reflected on their opinion of me.”
Madlove creates positive spaces to experience mental distress, bringing together people with lived experience, mental health professionals, academics etc to build the most-beautiful, craziest, bonkers asylum we have every dreamed of
Boredom is also a major problem for patients, with activity rooms containing little in the way of stimulation.
And Watson called on product designers to work with service users to create new solutions which would help to address these issues while creating environments that were more conducive to recovery.
“Different facilities take different approaches,” she told the conference.
“In my experience I prefer to use facilities more like I’m used to.
“In the community I would not expect to go to the toilet and have no door, for example.
“I understand there are risks and that observation needs to take place, but at the same time I think there’s ways around managing risk and still having a door.
“There’s enough innovation that this can be managed more effectively.”
Time for change
The conference also heard from James Leadbitter, the creator of Madlove: A Designer Asylum, a long-term project that blends research, design, building, and exhibitions to reimagine mental health support and the environments this support happens in.
In a hard-hitting presentation, he described many mental health units as ‘fugly places that make me want to die’.
I understand there are risks and that observation needs to happen, but at the same time I think there’s ways around managing risk and still having a door
And he said: “I have been in enough mental health hospitals to know something has to change, and that change is massive.
“Madlove asks ‘what if the places we need to feel safe in to experience our pain and to be made well were better designed and run by mad people, for mad people?’”
Launched in 2013, Madlove challenges the concept that mental health units are ‘more punishment and less love’.
Leadbitter said: “Madlove creates positive spaces to experience mental distress, bringing together people with lived experience, mental health professionals, academics etc to build the most-beautiful, craziest, bonkers asylum we have every dreamed of; unique spaces where mental care can be destigmatised and challenged and divisions between staff and patients can be understood and worked through together.”
Since its launch, Madlove has held workshops with more than 500 people with lived experience of mental health services and their families and carers.
A place for everything
“I met someone at one of these events in Ireland last year and they had been in and out of hospital for 30 years and said they were waiting for someone to ask them what their perfect hospital would look like,” Leadbitter said.
“It’s about what does good care look like, smell like, feel like and taste like.
“And everyone says the same thing, whatever setting, whatever age. “They want an environment on a human scale and run by people with lived experience.
“Spaces should be stimulating, not deadening, with light and music and silence and natural landscape, with somewhere to scream in or just to look at the stars.
“We want space for cinema rooms, and rooms with Faberge eggs and hammers, and smells which link to positive memories.
“People say it’s too risky or there’s no money, but I hope that by working together things will get better.”
Among the organisations Leadbitter’s team has worked with is Great Ormond Street Hospital, where they led workshops for children and young people with psychiatric conditions.
Everyone says the same thing, whatever setting, whatever age. They want an environment on a human scale and run by people with lived experience
During these sessions they asked children to put sticky notes on things they didn’t like within the environment – which included noisy machines, frames without pictures, and low roofs.
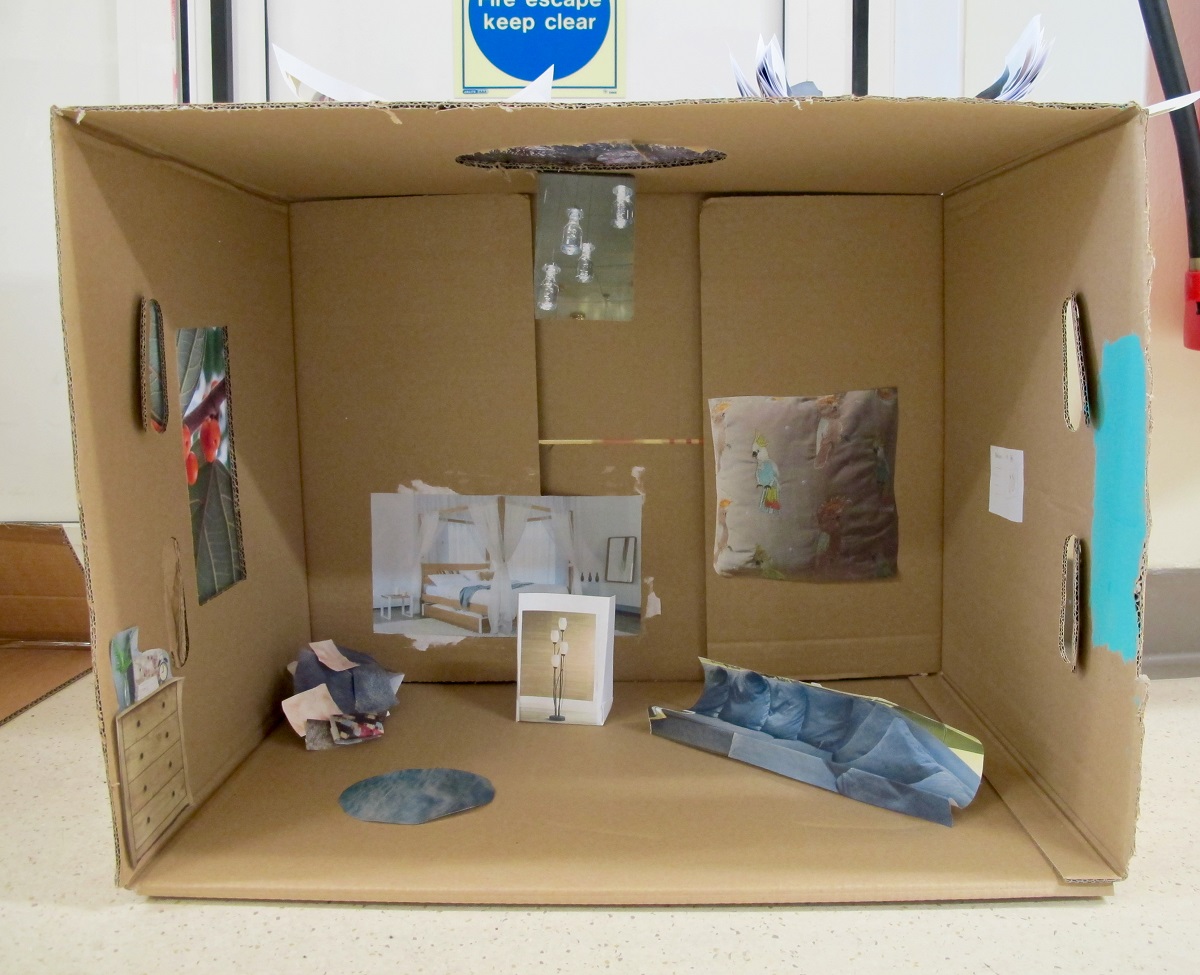
They were also taken shopping and asked to take photographs which were later used to create their ideal room design.
“We got them to redesign the whole ward and there were over 140 suggestions,” said Leadbitter.
Utopia is a process
“Children are smart, and they know what they want.”
He added: “For many people everything I have said might seem obvious, and it is really obvious.
“We are in pain, but we are not stupid. We have knowledge and you need to tap into that.
“Mental health hospitals have been around for thousands of years, but the focus is on protecting infrastructure rather than people and that will take time to change, but it has got to happen.
“We need to be smart about where we are directing resources. What we need are human beings, not doors and cameras and safety glass. It’s someone to ask if you’re OK.
“Utopia is a process and it’s a journey we will always be on, but I hope by working together it will get better.”